Why You Need to Know Your Breast Density
Breast density is an essential facet of women’s health that often isn’t as widely understood or discussed as it should be. I have to admit, as a woman who was always health vigilant and went for regular mammograms, I was unfamiliar with the term. No one ever talked to me about breast density. I recall a mammogram technician saying to me one time that my breasts were “ropey” but I never knew what that meant.
Just to confuse things even more, when I was diagnosed with breast cancer and understood the implications of breast density, I inquired about my breast density. I was informed by my family doctor that I did not have particularly dense breasts. That said, the surgeon who examined me at the time of my biopsy said that my cancer was hiding under an area of density. So I remain confused and no longer have boobs so will never truly know the answer to that question.
Back to the topic at hand, I also didn’t know WHY it is vitally important that women know their breast density. It is information that can save your life. So, ladies, why aren’t we all talking about it? And including our doctors?
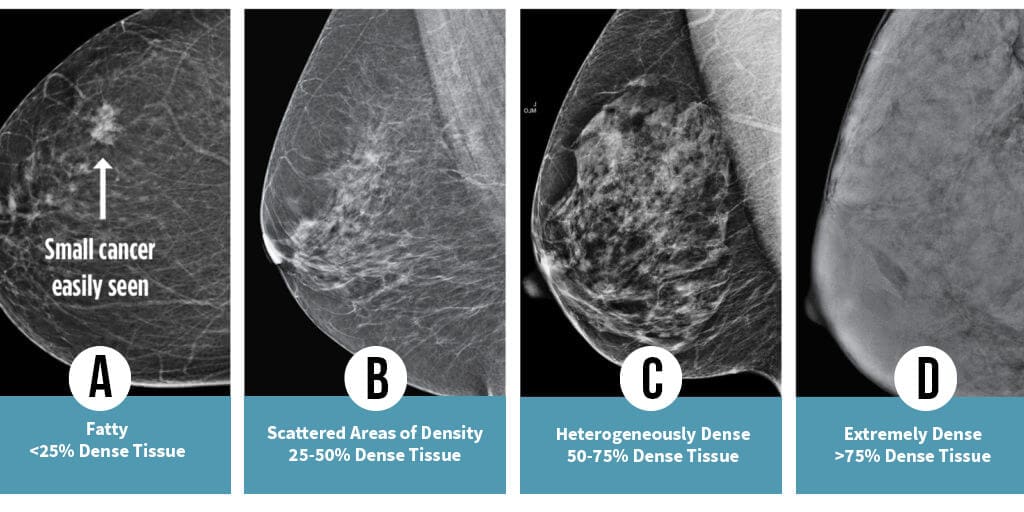
If you were to feel a denser breast, it might not seem very different from a less dense one. That’s because breast density is not about how a breast feels but how your breast tissue appears on a mammogram. Each woman’s breasts are a distinct mix of fatty and fibroglandular tissue. Dense breasts have more fibroglandular tissue, which appears white on a mammogram. Less dense breasts, on the other hand, have more fatty tissue, which appears black.
Understanding breast density is important because it can impact how breast cancer is screened and detected. Dense breast tissue can mask potential cancers on a mammogram because both dense tissue and cancer appear white, creating a ‘white-out’ effect and making the detection of breast abnormalities challenging. While mammograms are highly accurate in women with fatty breasts, their accuracy drops tremendously – to as low as 30% – in women with the densest, category D breasts. Recognizing this limitation is crucial for early detection and treatment.
Breast density, I should note, is pretty common. Research indicates that more than half of women in their 40s, and over a third of women in their 50s have dense breasts. But it’s not just the prevalence that makes this a significant issue. Women with the highest breast density are 4 to 6 times more likely to develop breast cancer. That’s a statistic we simply can’t ignore!
After a mammogram is performed, images are interpreted by the reading radiologist. Using the Breast Imaging Reporting and Data System (BI-RADS) a category of density is assigned ranking from from A (almost entirely fatty) to D (extremely dense). This density rating, found in the radiology report, can then be used to tailor your breast health strategy better. In the Province of Ontario Canada where I live, as of July 2023, this information must be shared with women. In April 2023 the US FDA also ruled that American women must be advised of their breast density, a ruling that goes into effect in 2024. Why this vital information was not mandated to be shared earlier is mystifying to me. But that’s an issue for a later blog.
Women with higher breast density (categories C and D) should receive additional screening methods, such as ultrasounds or if available, an MRI, due to the reduced efficacy of mammograms alone, but unfortunately this does not always occur. Further evidence that women need to have this information to advocate for themselves. .
Still, the journey to being informed and proactive about breast health doesn’t stop at understanding breast density and its implications. Women must have access to this information and be advised of their breast density, and provided the option of supplemental screening. By gaining this key piece of information, and having a clearly articulated pathway forward, women can better understand their risk profile and advocate for themselves. Sadly, doctors are still not proactively acting on this information. The onus is still on women to use this information to demand action from their doctors to be given access to supplemental screening beyond mammography. This too baffles me. Can you imagine a family practitioner not acting on abnormal bloodwork or a finding of high cholesteral? How is this different?
As an aside: If you know you have category C or D breast density and are receiving pushback from your doctor Dense Breasts Canada provides some scripts women can use in conversation with their doctors.
The goal is not to inspire fear, but to encourage awareness and informed action among women worldwide. Primarily, it’s about arming ourselves with knowledge – the knowledge of our own bodies, the understanding of our unique risks, and the power to ensure we’re receiving the best possible care. The stakes are simply too high to settle for less.
Further dialogue and advocacy are needed to ensure every woman worldwide knows her breast density. As I said at the opening of this piece, it is a conversation that can save lives. And sadly, we still have a long way to go before every woman is armed with this knowledge.
As a final word, remember always that breast density is an important factor, but only one of many risk factors for breast cancer. To have a truly comprehensive understanding of your risk it is recommended women perform a self-evaluation to gain a sense of their risk. And always, know your normal, do your self-checks and remain always breast aware.
Below are some excellent and credible resources that are Ellyn recommended if you want to dive more deeply into this topic.
https://densebreast-info.org/europe
https://www.breastcancer.org/risk/risk-factors/dense-breasts






One Comment
Pingback: