Managing stress after a breast cancer diagnosis is so vital, but also very hard. I vividly recall the way I felt after my doctor broke the news to me that I had breast cancer. It was my worst nightmare come true. I could barely breathe let alone think. I recall saying to my brother I felt like I had been simultaneously punched in the gut and had all the air sucked out of my lungs. In the four weeks I had to wait between finding out about my diagnosis and my biopsy (the thought of it terrified me), I lost close to 10 pounds. I had no appetite. My heart would pound nearly out of my chest. I couldn’t concentrate. In the evening I would curl up on the sofa in the fetal position and watch Shitts Creek (thank you Dan Levy). It was the only thing that would momentarily take my mind off what I was feeling and experiencing. My family were helpless bystanders to my emotional car wreck. My husband tried to console me but said all the wrong things. My friends tried to bolster me. Nothing worked in those early days.
But in time, I did discover some strategies to cope that I am happy to share in the hopes they also work for you. I’m not a doctor, nor am I a mental health professional. So these are just my personal experiences. Please consult a professional if you find yourself in similar circumstances.
Medication for Managing Stress
While I just said I was not thinking clearly, I did have the foresight to know that this was going to be a very difficult and rocky journey. So I advocated for myself with my family physician right at the time of diagnosis. She prescribed a small dose of anti-anxiety medication that I began taking immediately. I understand that pharmaceuticals are not everyone’s cup of tea or a panacea. That said, I have no shame in recognizing that I needed additional help to get through a difficult and emotionally stressful time. I continue to take the medication to this day. Go figure, I have probably always had high-functioning anxiety. And here I thought I was just a type A personality. Please note I am not a medical professional, please consult your doctor on all medical matters.
Therapy for Managing Stress
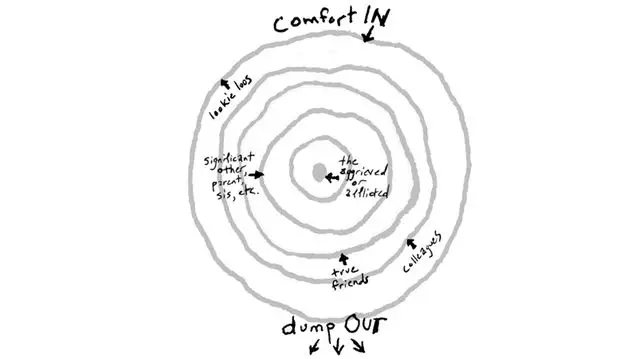
I also sought out the help of a therapist as a compassionate, professional sounding board. My family was as traumatized as I was (perhaps more so) and frankly, it would be unfair of me to unload my emotions on them, nor were they equipped to handle the fear and concerns that plagued me in those early days. I met regularly with a therapist, especially in the first few months as I processed my diagnosis, navigated appointments and the fear they brought, and news that seemed to get progressively worse. With her I could close the door to my office, express my innermost thoughts, and often, cry uncontrollably. She helped me understand the brain’s fright and flight response and gave me strategies to calm my parasympathetic nervous system. I have since also worked with a second therapist who specializes in trauma recovery as I try to process all that happened and navigate life after active treatment. I’m still an ongoing project in that regard.
Tapping for Managing Stress
I have a cousin who does a lot of work in trauma for an airline. She is a big believer in the tapping method. I have to admit, I regarded it all as a bit of a whoo-hoo thing — until I tried it myself, and after a couple of rounds, dissolved into gales of tears, allowing me to finally release all the emotion I had bottled up inside me.
As I have come to know, tapping, also known as EFT (Emotional Freedom Technique), is a powerful stress relief technique. Tapping is based on the combined principles of ancient Chinese acupressure and modern psychology. Studies have shown that Tapping decreases cortisol (often called the stress hormone) in your body. Sure you look a bit goofy going through the tapping routine, but I strongly recommend it now to women who are struggling in the early days of diagnosis. I will often even now return to this routine I found online when I need to settle. Just thinking about it now, I might just have to fire up the routine when I finish this blog.
Movement for Managing Stress
Movement and vigorous exercise have been a part of my life since I was in university. The endorphins released from exercise have always been a huge mood booster and stress reliever for me. My children when they were young used to say if I was particularly cranky, “mum have you exercised today?”
While other parts of me shut down, I continued to exercise throughout the early days of diagnosis, returned to it as soon as I was cleared after surgery, and yes, even during chemotherapy and radiation. There’s lots of research that shows exercise can alleviate and lessen the side effects of of cancer treatment. I was diagnosed in the spring and had treatment during the summer, so I did a lot of walking in addition to shadow boxing, free weights and pilates. I craved the outdoors and fresh air. I wore out the soles of my running shoes over this period, pounding the sidewalk as angry anthem music from P!NK blared from my earbuds. I will say, and I’ve written about it here, that exercise was instrumental in helping me cope and helping me heal well and quickly.
As I am still dealing with residual trauma, these days I have added somatic movement into my exercise regime, specifically doing up to 30 minutes a day of hip opening exercises. Again, probably something I should have been doing all my life as someone who spends her days either in forward motion or sitting at a desk. It’s been tremendously helpful in alleviating some long-standing hip stiffness and in releasing stored-up trauma.
Breathing for Managing Stress
The tapping routine I found online also incorporated deep breathing methods, which my therapist also recommended. The 4-7-8 breathing technique is a method that can help reduce anxiety and improve sleep. It involves breathing in for four seconds, holding your breath for seven seconds, and then exhaling for eight seconds. This technique helps to slow down your breathing and encourages your body to enter a state of deep relaxation. It works well now for me, but in the early stages when my emotions were running incredibly high, I found that this deep breathing technique on its own didn’t quite get me to a settled place. It wasn’t until I incorporated the ETF tapping in addition to breathing that I was able to let go and find relief.
Cold Compresses for Managing Stress
This was another strategy my therapist recommended to try to soothe and calm the parasympathetic nervous system when I was experiencing extreme anxiety or a panic attack (yes I had them). Icing the vagus nerve (which runs from your brain to your abdomen and carries emotions from the brain to the rest of your organs) is understood to be a way to quell anxiety by restricting blood flow. This can be a cold compress applied to your sternum, or in my case, I used to hold a bottle of ice water to my chest.
Meditation for Managing Stress
Meditation can be a powerful practice for managing anxiety. It can slow breathing, still the mind and reduce a racing heart. After I was diagnosed, I turned to breath-guided meditation as a way of curbing my anxious mind. A thoughtful friend of mine who taught yoga for years kindly sent me a practice she designed specifically for me. It was incredibly helpful for those times when I simply felt my world was caving in and I couldn’t get off the floor. I also used sleep meditation at bedtime as a way to calm myself. Sleep is health and restorative and meditation was a way of letting me clear my mind and slip away.
Massage
I had a group of friends who came together after I was diagnosed and gifted me several massage gift certificates. I put these to use in advance of every chemotherapy session. I’d book a 60-minute full body massage a few days before my infusion to relax, restore and recharge. Massage prior to chemotherapy has also has been scientifically shown to help alleviate and even prevent the onset of peripheral neuropathy. I will once again mention that I am not a doctor. While I did not have any issues with massage, there can be detrimental side effects for some individuals who are undergoing chemotherapy, so always clear it with your oncologist before booking time on the table.
3-3-3 Rule
Finally, my trauma therapist taught me the 3-3-3 rule to pull out in a pinch. I had a session with her where the tears would not stop flowing. When it happened on our call she had me look around, identify 3 objects and 3 sounds, and then move 3 body parts, and soon after the tears dried up and I was able to collect myself. The 3-3-3 strategy is a common tool in a therapist’s toolkit and helps one focus and ground oneself when anxiety seems overwhelming.