A guest post by Brigitte Roth
I had my bilateral mastectomy on Thursday, July 3rd at 8:00 AM (delayed from the original June 20th date because some pre-op appointments hadn’t been scheduled as required).
A bilateral mastectomy is considered a day surgery. My surgery took place at our local health center. All of the surgical staff were incredibly lovely. My nurse, who took me away to the OR, was so kind. He initially brought me just outside my operating room and said he’d return shortly when everything was ready.
Once in the operating room and hooked up to machines, my kind nurse squeezed my arm as my heart rate beat faster while I was waiting for things to start – and I said, to him (and to myself), “I know – calm down.”
My anesthesiologist was also great. He popped by while I was still in the day surgery area and asked me to show him how wide I could open my mouth, evidently for intubation to come (though he didn’t say that… he said “just for sizing”).
Into the OR for my Bilateral Mastectomy
In the operating room, he was so excited that I took a series of vitamins in preparation for my bilateral mastectomy surgery. I shared with him that I couldn’t take full credit, I only started taking the combination of vitamins following my cousins’ recommendations when I began chemotherapy. He said to me, “NO ONE takes these necessary vitamins!” They were important from his perspective.
For anyone interested, daily I take 120 mg K2 + 1000 IU D3; a Multivitamin for Women; 1200 mcg B12; 50 mg Zinc (as gluconate); and then, at bedtime: 200 mg Magnesium Bisglycinate.
The last thing I remember is an oxygen mask being placed over my mouth and nose, and the anesthesiologist asking me to breathe normally. Which I did. Then he said, ok, now deeper breaths. Two deep breaths later, I was out.
Hours went by without my knowledge.
On to the Recovery Room
I woke up at 11:50 in the post-anesthetic care unit (PACU) and by 12:30 PM, I was moved from the PACU to the day surgery area. I left for home by 2:15 PM.
From the surgeon’s report, I can confirm I had three doctors in the OR with me for my bilateral mastectomy: my surgeon, a surgical assistant and my new friend, the anesthesiologist.
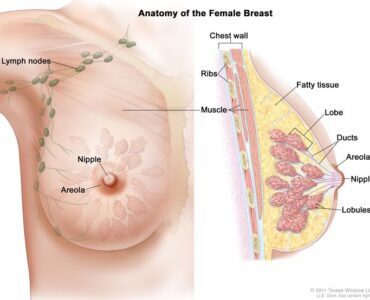
Once I was under anesthesia, 2 mL of blue dye was injected into the breast; this is in addition to Technitium 99, which was injected the day before during my nuclear medicine appointment.
The bilateral mastectomy surgery started by performing the right mastectomy. They then identified the cluster of lymph nodes (located by the blue dye and radioactivity), excised them and sent them off to pathology for “frozen section.” My surgeon was able to identify two additional sentinel lymph nodes (using the neoprobe). These were also excised and passed off to pathology.
While awaiting pathology results, they performed the left side mastectomy (no need for lymph node excision on the left side as my triple negative breast cancer was on the right).
Pathology called back, confirming there was a response from the neoadjuvant chemotherapy I had completed in the first phase of my treatment. So no axillary lymph node dissection was required (just the few taken out were enough — exactly the outcome I was hoping for, and evidence that chemotherapy does indeed work!
A pectoralis nerve block was performed for post-op pain control. It lasts 24 hours.
All sponge, needle and instrument counts were correct.
My estimated blood loss was 100 mL.
My right breast weight: 1511 g
My left breast weight: 1340 g
Back in day surgery, the nurse gave me some additional information and instructions to follow for the next couple of weeks as I recovered at home from my bilateral mastectomy.
Recovering at Home
• My surgical drains will remain in place for up to two weeks, or less if I am lucky. I have to see less than 40 mLs of output from each drain for two days in a row to have them removed.
- I could shower the next day and I did!
- I had a home care nurse come to my house today to remove the top dressing and replace the dressing at the drains. I learned the hard way they are not waterproof, so shallow baths for waist down – no showers – are allowed from now until drains are removed.
- Steri strips covering my incision areas will stay on for 7 days – they will likely fall off on their own. If they don’t, I’m to remove them on July 10
- I have to wear a sports bra or cami with a built-in bra 24/7 for two weeks for compression
- I should not engage in strenuous activity for four weeks
- I have pain meds of varying kinds (Tylenol, Advil, and some other narcotic) – so far, I have only taken one Advil yesterday.
- I should sleep with my arms above my heart for the first week. I have slept in an electric recliner both nights so far. I also have a surgery pillow for the bed, which I used part of the first night.
- I can use an ice pack as needed, 20 mins on/off – I’ve done it on/off sporadically so far
- I can’t submerge in a pool or bath for four to eight weeks (or until the incisions are completely healed)
- I can drive when I can turn my neck for blind spots (I already can!)
- I should do my functional rehabilitation exercises right away. These include ball squeezes, shoulder shrugs, head tilts, shoulder rotations and more, to ensure I regain full range of motion from my bilateral mastectomy and alleviate iron bra.
I have to say, I’m doing pretty darn well so far. I am very LUCKY. I’ve only experienced a couple of “zaps” of pain when I overextended (during sleep, trying to shift myself up in the recliner; and when I stretched to turn on the bedside lamp) and when I bent over to grab a frying pan. I can reach the first cupboard level, which is about at about my eye level, but not further up at this point.
Also, I had interesting bathroom colours from the injected blue dye – it was alarming at my first bathroom visit (no one warned me LOL) but got gradually less blue/green as the day went on yesterday.
Ironically, given everything, surgery was the most anxiety-provoking step for me, and it’s been so far so very good.
Only onwards and upwards from here.

Brigitte is a 51-year-old woman from Waterloo Region, Canada (and from a very large French Canadian family). She was diagnosed with Triple Negative Breast Cancer in the fall of 2024, only diagnosed through her very first mammogram in August that year. She started neoadjuvant chemotherapy mid December 2024 and completed her regimen in May 2025. Her bilateral mastectomy took place in July 2025.
Brigitte is owner of Acclaims Environmental, and most of her work relates to auditing drinking water systems and training drinking water operators in Ontario.